Valgus Knee [Case Study - Alec]
Background
At ONI we periodically go out to the public and ask for people to work with our specialists as case studies. The case studies have two main aims:
to help people live powerfully, without pain or injury.
provide a learning experience for the ONI team to apply the latest skills and strategies to real cases and real people.
February 2019 intake - Sarah A.
Sarah is one of our February 2019 case studies. Alec Morrison is working with Sarah to help with her knee valgus issues. The case study ran between 25 February to 1 April 2019.
A little bit about Sarah
she is doing a building apprenticeship
does a lot of physical activity both at work and outside of it, including going to the gym and mountain biking
has had no previous serious injuries.
What is knee valgus?
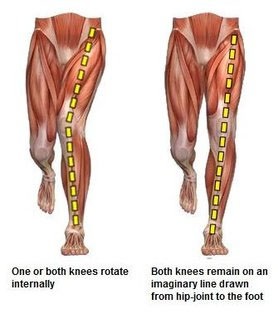
Knee valgus is also referred to as knock knee or knees caving in. It is characterised by hip adduction and hip internal rotation, usually when the hips are in a flexed position. It can also be thought of as knee caving as you sink down into a squat or landing.
How can it develop?
Knee valgus can occur for a number of reasons and a lot of the time several symptoms are present that contribute to this condition. These can include:
Weak hips
Weak or under utilised hip muscles, for (example glute medius and hip external rotators). It is also possible that weak hips in conjunction with overactive hip adductors, prevents proper stabilisation of the hip. The hips, in upright movements (like squatting and walking) would then move into adduction and internal rotation. When the adductors are overactive in comparison to the abductors, the knee is likely to be pulled into valgus.
Limited ankle mobility
Inadequate ankle dorsiflexion mobility (which may be due to joint restrictions as well as tight calf muscles: gastrocnemius, soleus), prevents the knee from moving forward efficiently and effectively. This causes the foot to compensate by pronating, forcing the knee to internally rotate, which leads to hip internal rotation and hip adduction, and therefore knee valgus.
Flat feet
Not having a proper foot arch means you are unable to absorb and transfer force when walking or doing movements like squats (which is why being fixed in either a flat footed position OR fixed in a high arch can be a problem, because both give you limited force production and absorption). Knee valgus is commonly associated with flat feet as the feet are in a caved in position where the knees tend to follow.
Sarah’s symptoms
Sarah said that she could not remember when she first felt like she had an issue with her lower body muscle structures. Sarah displays knee valgus when she walks (gait) and when doing movements like squats. She notes that she does not feel any pain or discomfort from this adaptation but feels the right leg is worse than the left. However, she notes that her friends, family and work colleagues have told her that the way she walks is very ‘distinctive’. She noted that the muscles in her inner thing (e.g. adductor longus and adductor magnus) are quite tight which are likely to be one contributing factor to her knee valgus.
Why would she show these symptoms?
As noted earlier, there are a number of factors that could lead an individual to display knee valgus. In Sarah’s case we were unable to pinpoint when this would have occurred however, it is likely that it is something that she has had for a long period of time. It is now her baseline movement pattern and is present when she walks, squats and when she undertakes other activities like climbing stairs etc.
Sarah’s goals
Over the six-week case study period Sarah wants to be able to do squats with good form and fix the knee valgus she has when walking. I explained to her that being able to squat in good form is a very achievable goal. However, it is likely to take much longer to change the way she walks. We agreed, that at the very least, by the end of the case study period she would have the tools to help improve her knee position when walking.
Assessment and analysis
- starting broadly and then narrowing in
Sarah understands that having knee valgus as a baseline position is something that could affect her well-being over time by putting unnecessary pressure through her knee (this could cause injury). At the start of the case study she was unaware of the muscles and structures that caused her condition and was interested to understand what they could be.
Broad test
Baseline position when walking
For my first test with Sarah I wanted to see what her baseline position was when she walked. I asked her to walk from one part of the gym to the other. The reason for doing this was to try and see Sarah’s knees valgus when she walks. The valgus was definitely noticeable and likely to be a compensation she has had for a long time particularly as she does not feel any discomfort when walking.
Squat pattern
Sarah, in her consult, noted that she found it hard to keep her knees from going into valgus when doing a squat. I wanted to see that first hand. I asked Sarah to perform a squat for me without any cuing. She again showed valgus in her knees and in particular a more pronounced valgus in her right knee. When doing the movement she struggled to maintain her balance. A lot of her weight was on her heels and there were times where it looked like she would fall. With some cuing she was able to do a better squat but again her knees caved in. The cues included having a more upright torso, having her arms out in front of her, trying to get her to move her knees in line with her feet.
Balancing on one leg
The next test we did was to see what compensations she made when balancing on one foot and in particular whether there was lack of balance shown in the foot or hip. When she got into this position she showed lack of balance in the hip. I made the decision to focus the next tests on narrowing in on the muscles and structures of the hip.
Narrow tests
After we went through the three assessments noted above we also wanted to test a few other areas.
Hip adductors
Firstly, as a quick test I got Sarah to get into a sitting position on the ground, I could clearly see when she was in the position that her adductor muscles looked shortened as she struggled to bring her knees towards her feet. I further tested my theory by getting her replicate this position while lying on the ground. Again, her legs struggled to lower toward the floor and were stuck at a higher than ‘normal’ range.
Glute medius
Secondly we tested her glute medius muscle. This muscle is responsible for hip abduction and external rotation (movements that help keep the knee from going into valgus). To test the functionality of the glute medius muscle I got her to perform a clam shell.
To get into this position she lay on her side, with her legs and feet together and had her legs raised to approximately a 70 degree angle. From there I got her to lift her knee while keeping her hips and feet in the same position. We then repeated the movement for the opposite side. Throughout the exercise, the glute medius was tested for activation through feel and questioning.
Initially, Sarah struggled to feel activation in her glute medius muscle and this continued until she felt tired and sore in the muscle. Her lack of feel and proprioception is likely due to the under use of the muscle.
Our approach to achieving Sarah’s goals over the six week period
Sarah’s main goal was to be able to perform a squat without showing knee valgus and also work towards improving her baseline movement pattern to not display knee valgus in her gait (walk). Our approach included strengthening and stability exercises, both bodyweight and with added resistance, to target weaker muscles as well as re-train movement patterns so that Sarah was able to achieve her goals. We worked hard together to achieve this as described below.
Pathway to improving her condition
- Sessional notes
Week 1
Week one included the consult and various assessments noted earlier. We also worked through two other exercises and some stretches which she also did at home and in the gym.
Exercises:
Description and cues:
Clam shell
We performed this exercise in the narrow test - note description in the earlier section.
Fire hydrants
Starting position is on your hands and knees. While in this position try and laterally lift your knee off the ground as high as you can while limiting movement in your hips or twisting your back.
Inner thigh (adductor stretch)
Stretching your inner thigh in a seated position with added pressure from your hands
Rationale for the exercises prescribed
As Sarah had underused hips and tight adductor muscles we wanted to strengthen her hips and loosen tension in her adductors. This was the focus for week 1 as well as getting Sarah to be able to activate her glute medius muscle and feel it contract.
As well as the consult, we worked on the following exercises during the session. They were also prescribed for her to do at home:
Twice a day (minimum) with a one day gap in between (e.g. Monday, Wednesday etc.)
Stretching your inner thigh in a seated position with added pressure from your hands - 4 times, hold for 15 seconds
Clam shell - 4 sets of 10 reps
Fire hydrants - 4 sets of 10 reps
Week 2
During the week two session we had a recap on the previous session and talked about how she went with the exercises at home and in the gym. Sarah noted that she unfortunately could only do her exercises twice during the week instead of three times. I explained to her that with conditions like knee valgus the more time she can dedicate to her treatment plan/exercises the better her results are likely to be.
She said that when she did do the exercises however, she was getting quite sore and tired in the glute medius muscle - something that we aimed to develop. She felt that she was able to feel and activate the muscle more than last week which was great progress.
She also said that she is now more aware of her knee valgus when she does other activities like walking and mountain biking. During these activities she said that she tried her best to move her knees into a better position. Unfortunately, she said that not only was this hard to do and maintain but it was also uncomfortable.
Exercises
Description and cues:
Clam shell with added pressure to the glute medius muscle from a mobility ball
Like last week this exercise was a clam shell but with added pressure/resistance from a small mobility ball.
Fire hydrant with isometric hold
Like last week but with a two second hold at the top of the movement.
Box squat
I got Sarah to do box squats. Her cues were to keep her feet tracking in line with her toes, keep her torso upright, try and keep her shoulders back and hold at the bottom (when she touched the box) of the squat for 2 seconds.
Paused box squat while catching and throwing a tennis ball
Same as above but pausing and maintaining her deep squat position while catching and throwing a tennis ball with alternating hands.
Rationale for the exercises prescribed
Sarah was able to feel the contractions in her glute medius slightly more than the week before. We wanted to continue to develop her control and feeling of this muscle. The added pressure from a mobility ball in the clam shell adds a little resistance for her to contract her muscles against which should ultimately lead to her feeling her muscle contractions. The isometric hold builds on the clam shell exercise but also adding the isometric hold should help with muscle endurance as Sarah noted that she felt quite tired in the glute medius when doing the exercises last week.
The two squatting exercises were a challenge for Sarah. A big focus of this session was to re-train the squat pattern and testing it by adding isometric holds and getting her to catch tennis balls to challenge her to hold her newly trained squat position.
The exercises below were prescribed for her to do at home:
Twice a day (minimum) with a one day gap in between (e.g. Monday, Wednesday etc.)
Stretching your inner thighs in a seated position with added pressure from your hands - 4 times, hold for 15 seconds
Clam shell with added pressure to the glute medius muscle from a mobility ball (or tennis ball) - 4 sets of 10 reps
Fire hydrant with isometric hold - 4 sets of 10 reps
Box squat - 4 sets of 10 reps
Week 3
We made it to half way through the case study period. Sarah had kept up with her exercises from last week and had found that she was able to do the movements more smoothly, and that she was stronger and more confident in her squat position. Sarah noted she was able to feel her glute medius muscle activate more on her right side (the side that displayed more pronounced knee valgus) than on her left.
We talked about progression and how we intended to increase the amount of resistance in her movements as well as adding in new movement patterns.
Exercises
Description and cues:
Adductor stretch
On your back, bring your knee towards your chest while maintaining a neutral spine. Hold this knee to chest position, unassisted, for 15 seconds each set. This also activates the hip flexors.
Standard bodyweight squats
Like last week but without assistance from the box.
Paused squat while catching and throwing a tennis ball
Again, same as last week but without assistance from the box.
Wall assisted stationary lunge
To help add another fundamental movement pattern to Sarah’s treatment plan I decided to get her to practice doing lunges. To do this I got Sarah to place a hand on a wall to help stabilise her as she performed a lunge. In the lunge I got her to stay as upright as possible and keep her knee in line with her toes as she lunged.
Rationale for the exercises prescribed
This week we wanted to add a little more resistance to her movements as well as learn a new movement pattern - the lunge. The beginning of the session still consisted of the clam shell and fire hydrant exercises we did the previous week. We made the fire hydrant slightly more challenging by placing a small band around her knees to add a little resistance to try and get more activation in her glute medius muscle. This extra resistance was found to be effective.
As Sarah was comfortable with doing box squats we decided this week to test if she could still maintain her good squat form without it. After very little cuing of keeping upright and pushing her knees out in the movement Sarah was able to squat without the assistance of the box. We also removed the box from the isometric hold and ball catching exercise.
The last addition to her treatment plan for this week was the lunge. Being able to lunge with good form and limited knee valgus should help in her being able to limit her knee valgus while walking. Next week we intend to integrate the lunge pattern into her walk.
The exercises below were prescribed for her to do at home:
Twice a day (minimum) with a one day gap in between (e.g. Monday, Wednesday etc.)
Stretching your inner thighs in a seated position with added pressure from your hands - 4 times, hold for 15 seconds
Adductor stretch - 4 times, hold for 15 seconds
Clam shell with added pressure to the glute medius muscle from a mobility ball (or tennis ball) - 4 sets of 10 reps
Fire hydrant with isometric hold - 4 sets of 10 reps
Squat - 4 sets of 10 reps
Wall assisted lunge - 4 sets of 10 reps
Week 4
This week I wanted to show Sarah how far she had come from when she first started the case study. In particular, to show that in four weeks through a structured plan significant changes to baseline movement patterns are possible. We first talked about her squat and how she is now able to not only perform the movement more efficiently but she has also increased aspects like her squat depth. When we talked through her progress she also said that it feels less awkward when she does the squatting movement (i.e. her new pattern is now her baseline) and that she feels that her gait has improved without any specific work on it.
As well as reflecting on how far she had come we also decided to add to the difficulty of the movements she was already performing.
Exercises
Description and cues:
Weighted squats
Continued with the squat pattern but while holding a kettlebell with both hands close to her chest.
Unassisted stationary lunge
Stationary lunge without wall assistance.
Walking in a straight line with limited knee valgus
Focusing on her gait with aim to change her baseline walking pattern.
Rationale for exercises prescribed
This week the changes to her exercises prescription were as follows. We continued to add more resistance to Sarah’s squat and also removed the assistance provided to movements like her lunge. By adding more resistance to her squatting movement pattern we were giving Sarah more of a challenge and also getting her body to experience what it was like with more stress placed upon it.
We progressed the lunge pattern from last week and removed the assistance she had from the wall. This made the movement more challenging and she now has to focus more on integrating aspects like balance into the movement. She initially found this quite tough as her body was not used to moving in this way, particularly without support. After the first few sets she started to get the hang of the movement and actually executed it quite smoothly.
As walking with limited knee valgus was one of her goals I got Sarah to try her hardest to limit her valgus as she walked in a straight line (over about 10 paces). She said that she found it quite awkward but was impressed with herself because she was able to maintain a better gait through limited cuing. I asked Sarah if she could try and integrate this new walking pattern in her day-to-day. We came to the agreement that she would try and walk like this when at home and too and from her truck at her workplace (i.e. when she fetches and puts back her tools).
The exercises below were prescribed for her to do at home:
Twice a day (minimum) with a one day gap in between (e.g. Monday, Wednesday etc.)
Stretching your inner thighs in a seated position with added pressure from your hands - 4 times, hold for 15 seconds
Adductor stretch - 4 times, hold for 15 seconds
Clam shell with added pressure to the glute medius muscle from a mobility ball (or tennis ball) - 4 sets of 10 reps
Fire hydrant with isometric hold - 4 sets of 10 reps
Weighted Squat - 4 sets of 10 reps
Unassisted lunge - 4 sets of 10 reps
Integrating her new walking pattern
Week 5
This was the penultimate week of the six week case study. Speaking to Sarah this week she noted that she wasn’t able to do her exercises during the week. We again discussed the importance of doing as much training of her new pattern as possible to enable the best results. Although she hadn’t trained I still wanted to progress her exercises particularly her lunge and further challenge her squat by adding more weight to the movement and getting her integrating this pattern in a crab walk.
Exercises
Description and cues:
Crab walks while catching a ball
Get into squat position, move from one side to the other while catching a tennis ball and maintaining good squatting pattern.
Banded stationary lunge
We attached a band around Sarah’s knee so that it would add resistance by pulling her knee toward her mid-line - creating valgus. This tension would occur throughout the movement pattern and Sarah would have to fight against this added resistance to maintain knee alignment.
Rationale for exercises prescribed
This week the changes to her exercises prescribed were as follows. We added even more resistance to Sarah’s squat (now she is holding a 12 kg kettlebell) and also got her to do crab walks while trying to catch a tennis ball. Sarah had been challenged by isometrically holding her squat position while catching a ball. Now we wanted to progress this movement by getting her to do a crab walk which gets her to hold her squat position while moving laterally. This was a big challenge and she said she could really feel her glute medius muscles as well as her quadriceps firing.
We progressed the lunge pattern from last week and added resistance to her knee by placing a band which pulls her knee towards her mid-line. This made the movement more challenging and forced her to push against the resistance to maintain knee alignment in the lunge. She initially found this quite difficult as her knee was not used to being pulled by a foreign object. After the first few sets she began to feel more comfortable.
The exercises below were prescribed for her to do at home:
Twice a day (minimum) with a one day gap in between (e.g. Monday, Wednesday etc.)
Stretching your inner thighs in a seated position with added pressure from your hands - 4 times, hold for 15 seconds
Adductor stretch - 4 times, hold for 15 seconds
Clam shell with added pressure to the glute medius muscle from a mobility ball (or tennis ball) - 4 sets of 10 reps
Fire hydrant with isometric hold - 4 sets of 10 reps
Weighted Squat - 4 sets of 10 reps
Crab walk - 4 sets of 10 paces (5 starting on the left leg and 5 on the right)
Banded lunge - 4 sets of 10 reps
Further integrating her new walking pattern
Week 6
For the final week of the case study we recapped on the progress Sarah has made, took some pictures of her movements and also progressed her exercises from the previous week. This week we added a twitch/pull to her banded lunge exercise and increased the amount of sets and reps for each exercise.
Exercises
Description and cues:
Banded stationary lunge with twitch/pull
This exercise was like last week but we added a twitch/pull intermittently while she did the movement. Her aim was to limit her knees caving in throughout the movement.
Rationale for exercises prescribed
We attached a band around Sarah’s knee so that it would add resistance by pulling her knee toward her mid-line - creating valgus. This tension would occur throughout the movement pattern and Sarah would have to move against this added resistance to maintain knee alignment. While having the band attached I added more resistance by twitching/pulling the band slightly. This movement provided extra feedback and further tested whether she could hold her lunge position. I was looking to see whether she made any compensations throughout the movement e.g. lift her foot off the ground, twisting her hips etc. Sarah executed the movement quite well but did note that she had to work even harder when doing the movement.
Conclusion
“I've recently finished taking part in a case study with Alec to help stop my knees from caving inwards when I walk. Alec was great to work with, very knowledgeable and easy to talk to and made the sessions fun. Within the 6 weeks my walking changed for the better hugely and I'm now even able to do squats properly and confidently. Would highly recommend.”
Sarah A.
In six weeks Sarah achieved her goal to squat with good form and is well on her way to not displaying knee valgus when she walks.
When Sarah and I reflected on her goals at the start of the six week training period, she was surprised that the knee valgus (that she has had ever since she can remember) has improved significantly from when she first started. She is now more comfortable with her new movement pattern and is using it whenever she can, including when she walks and when she mountain bikes.
Sarah, through this case study has the tools to enhance her squat and better her gait. Going forward, it will be up to her to continue her exercises and put the tools she has at her disposal to good use.
Review
On reflection, if this case study was to be repeated, the aspects I would have considered altering are:
More detailed testing to better determine whether flat feet was also another factor that caused Sarah to display knee valgus - this would include narrow testing of the feet and muscles associated with holding and maintaining the arch of the feet
Actively reflecting on how much progress Sarah had made on a weekly basis to improve buy-in, in the hopes it would get her to do the prescribed treatment plan more diligently.
Following on from the previous point, the exercise list grew to a point it may have put Sarah off the treatment plan. I could have substituted movements as they progressed, instead of adding to the list.
Aiming to increase the intensity of the treatment plan e.g. by adding more resistance or progressing through exercises faster.
Case Study Lead: Alec Morrison
Assist: Laurent Pang
ONI Personal Training | Massage Therapy | Nutrition Coaching